Save articles for later
Add articles to your saved list and come back to them any time.
London: Physician associates (PAs) without medical training are learning “neurosurgery on the job” as British medical colleges call “extraordinary” meetings over the use of the unregulated profession.
The non-medical staff have been operating on skulls and brains, amputating limbs and toes, and removing patient’s tonsils in British hospitals, among other procedures.
Afaq Ali Sartaj, a physician associate in neurosurgery at Royal Preston Hospital, said he had “zero training in neurosurgery or neurology”.Credit: Bloomberg
Afaq Ali Sartaj, a physician associate in neurosurgery at Royal Preston Hospital, told the Physician Associate Podcast that he had “zero training in neurosurgery or neurology” during his course to become a PA and it was “all on-the-job learning”.
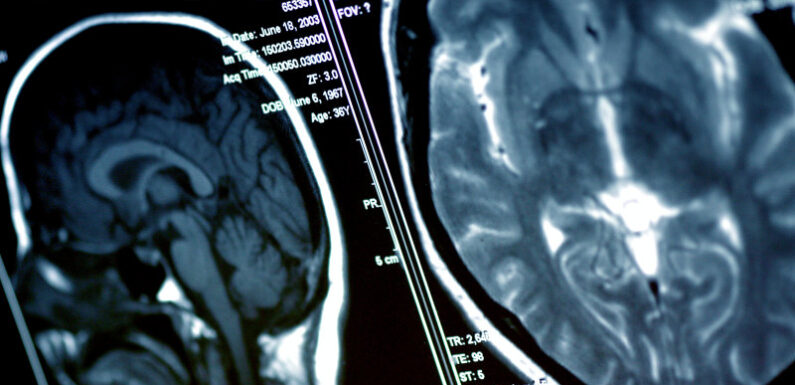
He now “scrubs in and operates on things like subdural haematoma evacuations”, which involves removing a pool of blood from a brain bleed after drilling a hole in the skull.
He regularly performs lumbar punctures and drains, which involve a small needle into the spinal cord to release pressure, and teaches junior doctors how to do them and “the insertion of intracranial pressure bolts – a small burr hole into the skull and then insert a little wire to measure the pressure.”
Sartaj said during “awake craniotomies” for tumours, where a surgeon removes part of the skull, he assesses patients’ speech and motor functions with tests to ensure the surgeon was not going too deep into the brain and risking permanent damage.
Another PA, currently in vascular surgery, went from working as a medical secretary to “co-operating major limb amputations” after undergoing a two-year postgraduate course.
“Under supervision I can perform toe amputations and alongside either a registrar or consultant I will co-operate in major limb amputations,” she told the Physician Associate Podcast.
“There have been cases where I’ve scrubbed in and opened a patient surgically and dissected down to a vein and harvested the vein for a bypass procedure.”
The PA, who works at University Hospitals Birmingham, said she was “training in endovenous surgical procedures” to treat varicose veins and had completed “a two-day course for ultrasound scanning” and a three-day surgical skill course alongside trainee surgeons.
The expanding use of the assistants has faced a backlash from doctors.
One doctor said it was “indulgence of an unregulated professional at the detriment of NHS patients”.
Another said “neurosurgery is classically one of the hardest and most rigorous training programmes in the country due to the skill needed and very high stakes”.
A separate Ear Nose and Throat (ENT) PA at Derriford Hospital in Plymouth, Molly Bowen-Jones, said she was learning to remove tonsils and insert grommets for paediatric patients with glue ear.
“An on-call day can be very varied, epistaxis, tonsillitis, lots of emergencies, airway emergencies,” she said.
“I’ve seen a lot of supraglottitis and epiglottitis in my short three years, which is always a little bit scary. You have to be able to do a flexible nasal endoscopy and that’s part of being an ENT.”
One of the main concerns doctors have is PAs not identifying themselves correctly, and the confusion this creates for the public.
Other examples included a urology PA conducting cystoscopies – bladder and urethra examinations – for cancer, while a PA in renal medicine said she removes kidney dialysis lines with an assistant such as “another junior doctor”.
PAs are unregulated but the General Medical Council is expected to oversee them from late 2024. They currently cannot order scans or prescribe medicine.
An A&E doctor said that a PA in the department had given him a prescription slip to approve 16 times the correct daily amount of tramadol – an opioid painkiller.
“You always have to keep on your toes,” he said.
An NHS spokesman said: “Physician associates are fully trained practitioners that support and work under the supervision of a consultant as part of a wider multi-disciplinary team at all times – they gain significant clinical experience during their training and can receive additional training throughout their career.
“They are internationally recognised roles which help to uphold the highest levels of patient safety while freeing up clinicians to spend more time with patients, enabling more people to get the care they need more quickly.”
The Telegraph, London
Get a note directly from our foreign correspondents on what’s making headlines around the world. Sign up for our weekly What in the World newsletter.
Most Viewed in World
From our partners
Source: Read Full Article
